.png?width=1024&height=512&name=Untitled%20design%20(6).png)
In the realm of healthcare, where patient safety and infection control are paramount, the meticulous sterilization of surgical tools plays a pivotal role. The re-sterilization of these instruments has emerged as a critical issue that demands our attention. This practice, while often driven by cost considerations, raises concerns about its potential impact on patient safety and infection control standards. In this blog post, we delve into the complexities surrounding the re-sterilization of surgical tools and the imperative for a thorough examination of its consequences.
The Basics of Sterilization
Sterilization is the process of eliminating all forms of microbial life, including bacteria, viruses, and spores, from surfaces and instruments. In healthcare settings, particularly during surgical procedures, the importance of sterile instruments cannot be overstated. Any lapse in the sterilization process can pose significant risks to patient safety, leading to infections, complications, and, in extreme cases, even mortality.
Understanding Re-Sterilization
Re-sterilization involves the repeated sterilization of surgical instruments for reuse. While the idea of cost-effectiveness is a driving force behind this practice, it introduces a layer of complexity and potential risks that cannot be ignored. The repeated exposure of instruments to sterilization processes may compromise their structural integrity, rendering them less effective in achieving the desired level of sterility. Additionally, the accumulation of wear and tear over multiple cycles may lead to the release of particulate matter, further escalating the risk of infection.
.png?width=900&height=600&name=Untitled%20design%20(10).png)
Risk Factors and Consequences
- Reduced Efficacy:
- Repeated sterilization cycles can compromise the functionality of surgical instruments. The heat, pressure, and chemical exposure involved in sterilization may lead to corrosion, blunting, or other forms of damage, reducing the efficacy of the instruments.
- Microbial Contamination:
- The very purpose of sterilization is to eliminate all microbial life. However, with each re-sterilization cycle, the likelihood of incomplete eradication increases, leaving behind potentially harmful microorganisms that can contribute to post-surgical infections.
- Material Degradation:
- Surgical instruments are often composed of sensitive materials that may not withstand multiple rounds of sterilization. This can result in the release of toxic substances or the deterioration of the instrument's physical properties.
- Regulatory Compliance:
- Many healthcare facilities adhere to strict regulations and guidelines regarding the use of sterile instruments. Re-sterilization practices must align with these standards to ensure compliance and maintain the highest level of patient care.
.png?width=1024&height=512&name=Untitled%20design%20(9).png)
Moving Forward
- Education and Awareness:
- Healthcare professionals must be well-informed about the potential risks associated with re-sterilization. This includes understanding the limitations of different sterilization methods and recognizing signs of instrument degradation.
- Investment in Quality Assurance:
- Allocating resources to invest in high-quality surgical instruments and state-of-the-art sterilization equipment can mitigate the need for frequent re-sterilization. A commitment to quality assurance is an investment in patient safety.
- Adherence to Guidelines:
- Strict adherence to established guidelines and regulations regarding the sterilization and reuse of surgical instruments is non-negotiable. Healthcare facilities must prioritize patient safety over cost considerations.
- Consider Single Use Surgical Instruments:
- Disposable instruments for certain procedures to eliminate the risk of infection transmission altogether.
Single-Use Surgical Instruments
Single-use instruments are designed for one-time use and are discarded after a single procedure. They come pre-sterilized, eliminating the need for re-sterilization and the associated risks. While they can be more expensive upfront, they can be cost-effective when considering the potential risks and costs associated with re-sterilization.
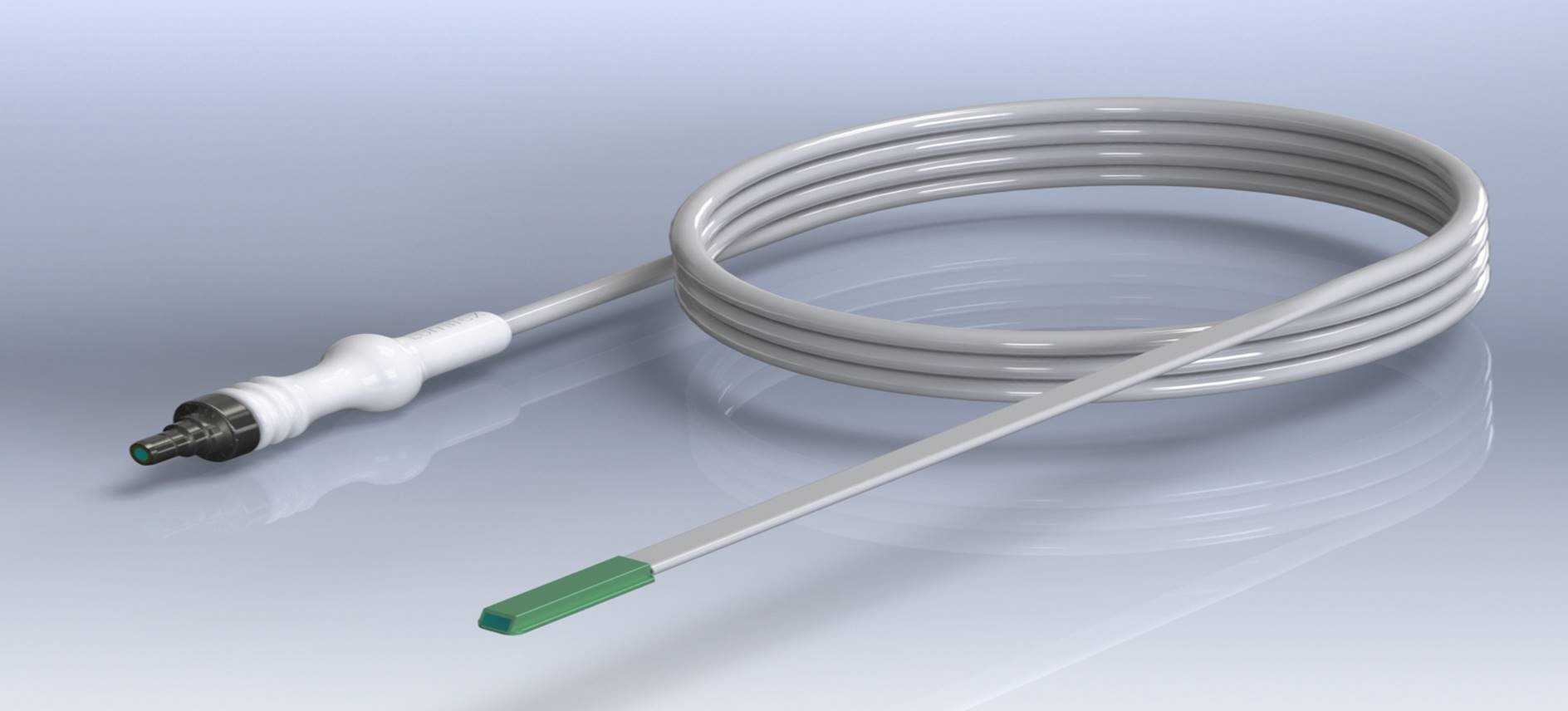
At Lumitex, advances in lighting will continue as technology and alternative options evolve. Our new design technology, Single Cable System (SCS) is one of the new advances. The single cable system delivers precise, in-cavity lighting from source to surgical site, eliminating the need for reusable intermediate cables. We always strive to concentrate on the quality of light and reflect that concentration through our technology.
Conclusion
The re-sterilization of surgical tools poses a significant risk to patients and healthcare facilities. In light of these risks, it is crucial for healthcare providers and policymakers to prioritize patient safety and consider alternatives to re-sterilization. The adoption of single-use instruments, improvements in sterilization processes, and increased regulatory oversight can collectively lead to a safer and more effective healthcare environment.
Frequently Asked Questions
How can re-sterilization affect instrument performance?
Exposure to repeated heat, pressure, and chemicals can cause corrosion, blunting, or structural damage, compromising the tools’ function.
Are there safer alternatives to re-sterilization?
Yes. Single-use surgical instruments eliminate the need for re-sterilization, come pre-sterilized, and reduce the risk of infection.
How does Lumitex’s Single Cable System (SCS) relate to this issue?
The SCS provides precise in-cavity lighting without reusable intermediate cables, reducing contamination risks and aligning with safer, more efficient surgical practices.
References
- Michelle J. Alfa (2019) Medical instrument reprocessing: current issues with cleaning and cleaning monitoring, American Journal of Infection Control.
- Rechtsanwälte Dierks & Bohle, Berlin [Legal aspects of reuse and re-sterilization of disposable products in the hospital].
- Rutala WA, Weber DJ. Disinfection and Sterilization in Health Care Facilities: An Overview and Current Issues. Infect Dis Clin North Am. 2016 Sep;30(3):609-37. doi: 10.1016/j.idc.2016.04.002. PMID: 27515140; PMCID: PMC7134755.
- Ottardi, C., Damonti, A., Porazzi, E. et al. A comparative analysis of a disposable and a reusable pedicle screw instrument kit for lumbar arthrodesis: integrating HTA and MCDA. Health Econ Rev 7, 17 (2017).
- Guidance 1 on Enforcement Priorities For Single-Use Devices Reprocessed by Third Parties and Hospitals. J Clin Eng. 2000; 25: p 341–9.
- Medical Devices Agency. Single‐use medical devices: implications and consequences of re‐use. Med Devices Agency Device Bull. 2000;4:1–9.
- Decontamination and Reprocessing of Medical Devices for Healthcare Facilities. World Health Organization and Pan American Health Organization (2016).




Comments