
When designing a safe medical device for patients and users, several factors must be considered. Specifically, in the case of surgical lighting, there are critical risks to be mitigated, especially when the light source is near the patient's body during minimally invasive procedures.
In this article, we will discuss four major areas of safety concerns involving surgical lighting:
- Thermal safety
- Eye strain of medical staff, and
- Infection rates associated with reprocessing devices
- Power outages and lighting failures
We’ll review design concerns and how to overcome these challenges.
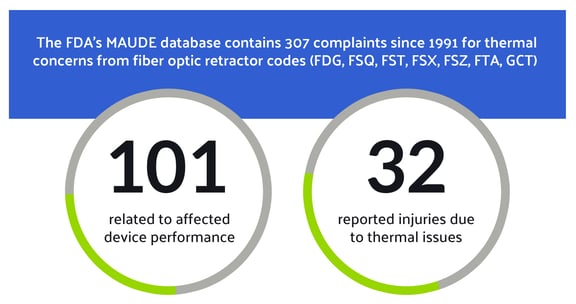
Thermal Safety
Applying electrical power to a medical lighting system typically results in heat transfer. Managing the transfer of heat is an important consideration in medical lighting design. When light hits an object, photon energy converts to thermal energy. With high-output lighting, as often seen in the operating room, there can be a lot of light absorption by various materials and patient tissues. The closer an intense light source is to the patient, the greater the concern for potential thermal injuries or burns. While, these types of injuries do not often happen with overhead lighting, they can occur more often with devices that emit light in close contact with the patient. Fiber optic retractors are surgical illumination devices used in minimally invasive procedures, and some fiber optic materials carry the risk of thermal injury to patients. Fiber optic lighting is typically provided by a standard operating room light source. Operating room light sources can vary by wattage, bulb age, bulb type, and infrared filtering, all of which affect thermal output. The FDA’s MAUDE database contains 307 complaints since 1991 for thermal concerns from fiber optic retractor codes (FDG, FSQ, FST, FSX, FSZ, FTA, GCT). Of those complaints, 101 are related to thermal concerns that affected the device performance, and 32 complaints are reported injuries due to thermal issues (between 2011-2021).
Tips for Optimal Performance and Thermal Management
There are several ways to improve the safety of fiber optic light sources, including lighted retractors.
- Halogen lamps produce lower heat output than xenon sources because they are typically less intense (1). LED light sources tend to require less power and they have significantly less output in infrared wavelengths; however, they can still present thermal risk with highly concentrated light. It’s not always possible to control the light source available in the OR, so when testing fiber optic lighting for thermal, always evaluate the worst-case scenario and recommend the best.
- Minimize the light intensity that also provides optimal visualization (1,2)
- An endoscopic ear surgery study shows that the clinical setting for output is 30% for xenon and 40% for LED (1). This means that comfortable viewing and achieving diagnostic visibility is possible at 30% of maximum intensity for a xenon light source, and diagnostic visibility is possible at 40% of maximum for LED sources. Endoscope tips remained below 31℃ when the appropriate intensity was selected but rose to 110℃ for a 4 mm endoscope at 100% intensity (1). End users should be encouraged to properly dial in their light source intensity, regardless of the fiber optic equipment used.
- Avoid direct contact with materials and the patient when using OR lighting instrumentation (3). Keep surgical light sources turned OFF when not in use, and place connectors on instrument trays rather than drapes or patient skin. Even overhead lighting and headlamps can cause thermal injury when positioned too close to a patient (4).
- The two most common types of fiber optic materials are glass and acrylic. Glass has a higher thermal transfer coefficient than acrylic and will allow more heat to be transferred from the light source to the patient. Due to their low thermal stability, acrylic fiber optics must operate at lower light intensity levels but are much safer for contact at the distal end. The lower output can be overcome if the lighting system is designed to appropriately filter and dissipate the heat at the proximal end near the light source. This allows light to escape as heat safely before reaching the patient.
- Safety standards have been increasing for endoscopic light sources (IEC 60601-2-18:2009, BS EN 60601-2-18:2015, IEEE 11073). Infrared filtering of halogen and xenon sources reduces the amount of heat transmitted from the bulb, while a fan removes heat quickly and efficiently away from staff and patients.
- Read the IFU (Information For Use) Documents that accompany fiber optic devices. Companies invest time and resources into testing to develop recommended best practices for using, maintaining, and storing devices to prevent malfunction and injuries.
Eye Strain of Medical Staff
One of the frequent user requirements and recommendations by guidance documents is that the light output for detailed tasks has very high illuminance levels. With high illumination, there are additional considerations for minimizing eye strain.
Eye strain for operating room staff is a safety concern to be addressed when incorporating lighting into surgical sites. The reason for using surgical lighting is to improve visibility during an operation, thus reducing eye strain. When operating room personnel are free from fatigue, procedures are faster and more accurate. A study by Hemphala et al. showed that 59% of OR medical personnel reported eye strain from their normal daily tasks. Those who reported eye strain were also 4x more likely to report other musculoskeletal discomfort, such as neck and shoulder pain (5). This musculoskeletal pain is due to compensating postures to reduce eye strain, such as extending the head for better visualization, which places extra strain on the neck and back muscles. 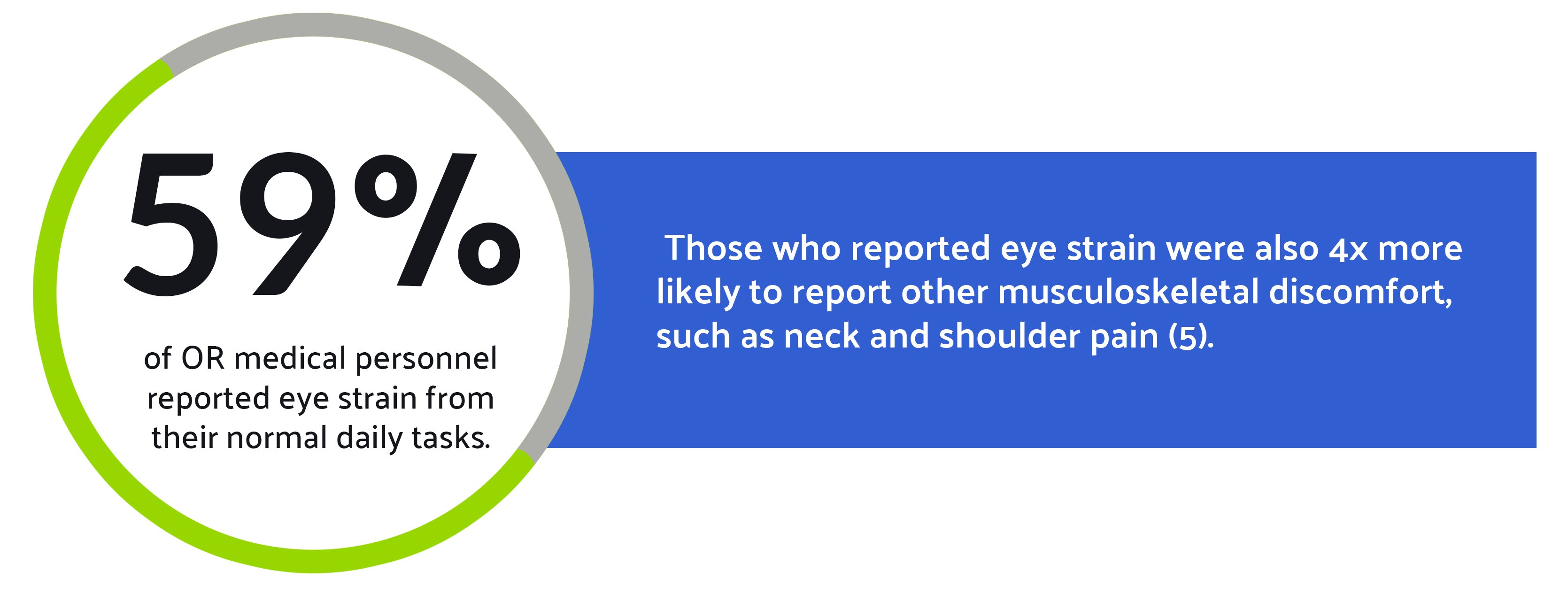
Eye strain can result from several factors, but two large causes are glare and pupil adaptation. Pupil adaptation and continuous re-adaptation due to high luminance ratios cause eye strain. Glare results in eye fatigue due to affecting visual ability (retinal bleaching). While it is true that more light is required for detailed work and greater illuminance is needed by aging eyes, too much contrast between workspaces leads to eye strain.
Preventing Eye Strain and Glare: Optimizing Luminance Ratios and Spectral Output in Surgical Lighting
Contrary to popular belief, more light is not necessarily better, especially when there is a high difference between task and ambient lighting. This difference is referred to as the luminance ratio. Luminance ratios have been well studied. IESNA Illuminating Engineering Society of North America recommends illuminance ratios of 3:1 between the operating cavity and the surrounding field and 5:1 between the cavity and the instrument tray (5). Too high of a luminance ratio results in eye strain and glare. The Hemphala study showed that greater central luminance resulted in faster visual acuity tests and better-perceived acuity. However, the time for eye adaptation to occur in the high luminance ratios (very bright central luminance, lower surrounding luminance) took up to two minutes for blurring and reduced image quality to subside. This is unlikely to affect surgeons if their focus does not deviate from the surgical site but can be an issue for circulating nurses and scrub nurses as they shift their visual focus between the OR site and peripheral sterile fields for instrumentation, etc. (5) It can also be a challenge for the anesthetist to shift focus between monitor screens and the patient. When considering a surgical lighting system, paying attention to the luminance ratios of the task lighting and the ambient lighting will help alleviate eye strain due to pupil adaptation. For example, screen lighting levels for a patient monitor might be adjustable for staff comfort in an OR with the lights dimmed versus brightly lit spaces.
Glare is a challenge due to the possibility of retinal bleaching. This is the phenomenon where a visual blind spot persists after the retina is exposed to too much light. It takes about 1-2 seconds for the eye to return to normal after glare, though this time can be extended depending on the severity of the glare (6). It also takes longer to recover from glare exposure as the eye ages. Beyond excessive light, subjective discomfort tends to be higher when the light's correlated color temperature (CCT) is higher. That is, the bluer the light appears to be, the worse the glare exposure tends to be (5). By keeping the spectral output balanced without excess blue wavelengths, glare can be less severe. Using the correct amount of light and a balanced spectral output can help alleviate the subjective discomfort caused by glare. More on color rendering and CCT is discussed further in our 2022 surgical lighting article (7).
Infection Rates Associated with Reprocessing Devices
Now that we’ve achieved reliable, safe lighting that allows clinicians to complete the procedure, the last piece is to choose proper sterilization techniques that are compatible with each medical device.
Appropriate sterilization and disposal of single-use medical devices are critical as it lowers infection rates caused by surgical site infections (SSIs). Surgical site infections are among the most common healthcare-associated infections (HAIs). The three types of surgical site infections described by the CDC are as follows (8):
- Superficial incisional SSI is when the infection occurs only in the skin where the incision was made.
- Deep incisional SSI is when the infection occurs underneath the incision area in muscle and tissues surrounding the muscles.
- Organ or space SSI is an infection in any area of the body other than the skin, muscle, and surrounding tissue involved in the surgery.
Addressing Reprocessing Challenges to Prevent Surgical Site Infections
SSIs mainly occur due to the inadequate reprocessing of medical devices. According to the Challenges of Medical Device Reprocessing report, 22% of all surgical site infections are related to equipment reprocessing (9). Some sterilizing methods and techniques can cause damage to medical equipment, which could pose a threat to patients’ health. One of the common sterilization methods used by healthcare facilities is Ethylene Oxide (EtO). EtO uses sterilant gases that are known to be toxic and carcinogenic, thus posing harm and risk to patients if devices are not accurately aerated. However, ETO is a very common and adaptable form of sterilization and does not cause damage to instruments (10).
Another method that could impact patients’ safety is the high-temperature sterilization technique. While many modern-day devices are unsuitable for high-temperature sterilization, some are considered compatible. However, over repeated exposure to high temperatures required for the sterilization process, the efficacy of such devices could be reduced, thus putting patients at risk. While ensuring patients' safety is of utmost importance and should be prioritized, it is also essential to consider the expenses associated with the high-temperature sterilization process, such as energy and water usage, as well as the need for premature replacement of equipment due to damage.
Reprocessing medical devices labeled as single-use devices (SUDs) is a practice that has been common over the last couple of years to save costs. Over a quarter of hospitals in the US and about 80% of hospitals in Spain reuse single-use devices (11). Although the FDA requires third-party reprocessors in the US to meet the same standards as the originally manufactured SUDs, improperly reprocessed items/devices such as needles, syringes, and catheters could cause serious infections such as HIV as well as hepatitis B and C. OEMs are implementing efforts to stop the adoption of reprocessing SUDs. Devices designed by OEMs have specific guidelines and labels that should be followed to ensure the safety of end users and patients. To be able to reprocess a SUD, OEMs must provide instructions on how to safely and properly sterilize reusable equipment when distributing; therefore, it is not safe enough to reuse medical devices labeled as single-use as it will increase infection rates.
As new sterilization technologies evolve, product design will need to consider product durability in terms of heat, chemical and mechanical resistance.
Power Outages and Lighting Failures
When thinking about a patient’s safety in an operating room (OR), it is important to remember and consider maintaining electrical power, as it is a huge factor in successful surgeries. Power failure in operating rooms is a serious event that requires acknowledgment and preparation as it can have severe consequences, potentially resulting in harm to patients and even life-threatening conditions. Unfortunately, like many other fundamental infrastructure elements in the world, uninterrupted electrical power may be taken for granted and is only given real attention when it’s absent (12).
An important element requiring a consistent power supply in an operating room is lighting. Proper and high-quality lighting is necessary for the OR, and all surgeries depend on it, whether lighting is overhead or in-cavity. Surgical lighting is a foundational component of safe surgical care and is classified by the World Health Organization (WHO) Service Availability and Readiness Assessment (SARA) as essential electrical equipment, falling under the following categories: infrastructure and support appliances for health services (13).

With the constant change in weather conditions and uncontrollable regional disasters, power outages are becoming more common and are mainly experienced in low-resource settings. According to a study of eleven sub-Saharan African countries, “only 28% of health facilities and 34% of hospitals had reliable access to electricity, defined as no outages for more than two hours in the past week” (13). This issue severely impacts surgical lighting and puts patients at risk. Many surgeons in high-resource settings wear specifically designed headlights to improve illumination. Such headlights are costly and are limited in low– and middle-income countries (LMICs) (13).
Moreover, due to poor surgical lighting when electrical power failures happen, surgeons must make tough decisions that introduce high risk to patients, such as delaying or canceling operations. Although most hospitals carry backup generators, a study by The Lifebox Foundation describes that only 48% of respondents noted that a backup generator would always be available. Besides relying on backup generators, it is also reported that 29% use mobile phone flashlights during power outages (13).

Preparing for Power Outages
Despite how common or uncommon the loss of power supply to the operating room is and the failure of backup generators, healthcare providers should prepare for such events as they would for any other crucial event that impacts patient safety. Preparing for such an event could include regular checkups and maintenance on backup systems as well as following specific protocols that are well understood by healthcare providers and OR assistants.
Medical device manufacturers should be aware of this and consider power outages when designing lighting for their medical devices. This intentional design is important as it helps reduce patient risk if the correct implementations were taken during the manufacturing process. One approach is having medical devices with 1-2 hour battery backup. Another is reducing power consumption needed for medical devices. This could help when a power outage occurs since the generators’ power capacity is limited. Also, choosing energy-efficient lighting technologies such as LEDs and CFLs over halogen lights could help minimize power consumption.
Conclusion
When designing a surgical lighting system, there are several factors that must be taken into account to mitigate potential risks. The primary concern should always be the safety of the patient, which can be ensured by creating a reliable lighting system and managing heat effectively. Additionally, it is important to provide clinicians with tailored lighting to optimize their performance during surgeries. Another critical consideration is device sterility and reprocessing to maintain the safety of the lighting system. Overall, these requirements are just a few of the many necessary design elements for creating an optimal surgical lighting solution.
- Ito, Tsukasa et al. Safety of heat generated by endoscope light sources in simulated transcanal endoscopic ear surgery. Auris Nasus Larynx 43 (2016) 501- 506
- Prasad, Navin et al. Thermal injury to commo operating room materials by fiber optic light sources and endoscopes. Am J Otolaryngol 40 (2019) 631-635.
- Nizzero D, Deek R, Dean NR. Prevention of thermal injury from lighted retractors in breast surgery—a comparative study of optical cable calibre. Australas J Plast Surg. 2022;5(1):39–42. https://doi. org/10.34239/ajops.v5n1.289
- Lupkin, Sydney. “Patients get ‘Burned’ during surgery at Oregon Hospital”. https://abcnews.go.com/Health/patients-burned-surgery/story?id=28434559. 23 Jan 2015.
- Hemphala, et al. Towards better lighting recommendations for open surgery. Lighting Res. Technol. 2020; 52: 856-882
- Prasad, Navin et al. Thermal injury to commo operating room materials by fiber optic light sources and endoscopes. Am J Otolaryngol 40 (2019) 631-635.
- Toich, S. (2022, September 20). Surgical lighting to optimize and focus light intensity. Lumitex. https://www.lumitex.com/blog/surgical-lighting-ergonomics
- “Surgical Site Infections.” Surgical Site Infections | Johns Hopkins Medicine, 22 Nov. 2019, https://www.hopkinsmedicine.org/health/conditions-and-diseases/surgical-site-infections
- ASP. https://www.asp.com/sites/default/files/pdf/AD-190028-01-CT_A%20ASP%20Ebook%20-%20Challenges%20on%20Medical%20Device%20Reprocessing.pdf.
- Shah, S. B., & Bhargava, A. K. (2017, October). Recent advances in low temperature sterilization - moving ahead from CIDEXTM/ETO to Opa/ozone: An update. Indian journal of anaesthesia. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5664899/
- “Are Reprocessed Single-Use Medical Devices Putting Patients at Risk?” NS Medical Devices, 16 June 2020, https://www.nsmedicaldevices.com/analysis/patient-risk-reprocessed-single-use-medical-devices/.
- Suh, et al. Anesthesia & Analgesia, https://journals.lww.com/anesthesia-analgesia/pages/default.aspx.
- Adair-Rohani H, Zukor K, Bonjour S, Wilburn S, Kuesel AC, Hebert R, Fletcher ER. Limited electricity access in health facilities of sub-Saharan Africa: a systematic review of data on electricity access, sources, and reliability. Glob Health Sci Pract. 2013 Aug 14;1(2):249-61. doi: 10.9745/GHSP-D-13-00037. PMID: 25276537; PMCID: PMC4168575.

Sara Toich
Sara Toich is a design engineer at Lumitex. She develops surgical lighting from ideation through design controls to production release. With a background as a veterinary orthopedic & spine surgical technician, she understands the challenges & importance of medical lighting. Sara is a Registered Veterinary Technician with a Bachelor of Science in Biomedical Engineering from the University of Akron.

Riham Alabed
Riham is one of the design engineers at Lumitex. She works closely with the surgical team to understand our customers' needs and develop products from ideation to release. Riham has a Bachelor of Science in Biomedical Engineering from the University of Akron.





Comments